| |
Strange as it may seem, the
brain itself is not sensitive to pain. There are no nociceptors
in the brain tissue, which explains why most brain surgery is done using local
anesthetic alone, to numb those tissues surrounding the brain, such as the meninges,
that are in fact sensitive to pain. |
The nociceptive neurons and their
axons maintain a somatotopic organization along their entire
length. From the spinothalamic
pathway in the spinal cord to the thalamus and on to the somatosensory cortex
in the brain, what is contiguous in the body generally remains contiguous all
the way up to the brain. It is this organizing principle that lets you locate
pain—for example, to feel it on precisely the toe that you have just stubbed.
A somatotopic organization is also found in the primary
motor cortex, but this organization is not fixed for all time: it can
be altered through training. For example, when a violinist practices for years
to improve the dexterity of her fingers, the area of the primary motor cortex
that maps to each finger is larger and better defined than in the average person.
| | |
When you stub your toe
on a rock, you feel a pain at that specific spot on your body. The pain is often
so sharp and so localized that you might be tempted to believe that it’s
your toe itself that’s experiencing the pain. But that’s not really
the case at all. First the nociceptive
fibres in your toe send nerve impulses to your spinal cord, which relays them
to your brain. And it is the neural activity of certain parts of your brain that
then makes you feel the pain in your toe, jump back from the rock, shout a few
choice words, and rub your toe vigorously. What are
these parts of the brain, and how do they work together to make you feel the multiple
properties of pain, such as the type
of pain and its location, intensity, and negative emotional charge? These
are complex questions that have been hotly debated over the past few decades and
continue to be so today.
Reticular
formation (red), ventral posterolateral nucleus (VPL) of the thalamus (green),
and somatosensory cortex (blue) | But
one thing seems certain: there is no single “pain centre” whose activity
alone could account for all the multiple aspects of pain. In other words, there
is no one part of the brain that could be surgically removed to eliminate all
pain. That said, experiments conducted with brain imaging and other technologies
do clearly show that when you are experiencing pain, the activity of many specific
areas of your brain is altered. These areas are interconnected and form a network
that some neuroscientists call the pain
matrix. And from what is already known about these areas, they are often associated
with different aspects of pain. | One
such area, located in the brainstem, is the reticular
formation, one of the first brain structures that receives connections
from the ascending
pain pathways in the spinal cord. The activation of the reticular formation
contributes to the reactions of awakeness and alertness associated with pain.
The neurons of the reticular formation can alter your heart rate, arterial blood
pressure, respiration, and other vital functions that can be affected by pain.
It is also the reticular formation that allows a pain stimulus to go unnoticed
if your attention is focused on some compelling task. The
next stop along the ascending pain pathways is the thalamus,
a brain structure that acts like a giant switchbox for sensory signals. There
the pain pathways make connections to various sub-regions of the thalamus, in
particular the ventral posterolateral (VPL) nucleus, which, as its name implies,
is located in the ventral, posterior, lateral portion of the thalamus. The
VPL nucleus then plays a major role in the sensory discrimination of pain. Its
neurons project their axons into the somatosensory cortex, a brain structure known
for its ability to locate pain and assess its intensity. Signals for the sense
of touch also pass through the VPL nucleus and on to this same cortex, but information
about pain and touch is handled in separate subregions of this nucleus. The
medial portion of the thalamus also receives connections from the reticular formation.
This part of the thalamus displays a more tenuous somatotopic organization (see
sidebar) that prevents it from playing as much of a role in discriminating the
bodily location of a stimulus. The neurons of the medial thalamus make connections
to the motor
cortical areas of the frontal lobe, whereby this part of the thalamus plays
a role in generating the motor and emotional reactions associated with pain.
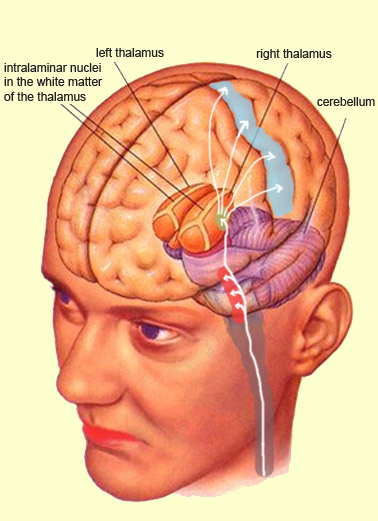
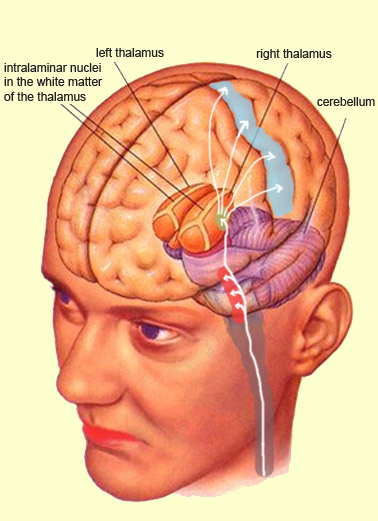
The intralaminar
nuclei of the thalamus, located quite close to the medial portion, are also
part of this “non-specific” area of the thalamus, which participates
in the alertness response to pain. In addition to connecting to the frontal lobe,
the intralaminar nuclei also project to various
parts of the limbic system. And because the frontal cortex itself sends numerous
projections to the limbic
system, these two structures taken together with the intralaminar nuclei unquestionably
constitute a system that is involved in the unpleasant emotional component of
pain and the behavioural responses designed to reduce it. Once
nociceptive messages reach the cerebral cortex, the abundance of reciprocal connections
there make the path of these messages much harder to follow. But brain-imaging
studies have confirmed that the primary
and secondary somatosensory cortexes, as well as the anterior cingulate cortex
and the insular cortex, are all involved in the perception of pain. |
|